Bryan a GP at a medium sized community practice, which uses MedTech32. He originally trained and briefly worked as a GP in the UK, but moved to New Zealand 11 years ago.
The unique thing about Bryan is his obsession with process.
"I am crazily obsessed about process. That's why none of my quality markers are missing, everything is filled in it's all done."
Every part of his workflow is incredibly considered and consistently followed. For every single process he does, he tries to shave 5 minutes or 5% of effort off it. This reduces his accumulative workload, and therefore he's always more likely to be ahead of the game, and not catching up on work.
"One of my abiding memories were how GPs were always running behind time, I realised in many ways we were just not working efficiently as a profession."
Bryan uses a large 24" monitor for MedTech32, and a secondary monitor for email, iMessage, browsing the web, and post it notes. For input, he uses a mechanical keyboard with no letters on the keys - he avoids using the mouse as much as possible. He used voice dictation software for a few years, but found that it doesn't do a perfect job, and notes would require proofreading - which was undermining any time saved by using it.
Bryan noticed when he first started working in New Zealand, MedTech's tab system. To swap between sections of the patient record, you need to open that specific tab. If you don't open the tab, you'll never know what's in there, or not. He found that many people wouldn't have drug allergies filled in, because they weren't in the exact spot. It was probably noted in the main body of the consultation notes, but not in the exact 'drug allergies' tab.
Viewing this as a downside, Bryan found that MedTech32 would allow you to open all tabs at once, and arrange them as you'd like. He prefers this at it lets him visually see all of a record at a glance, giving him a quick overview.
"I have figured out ways to overcome the problems with MedTech, but that's only because I'm a little bit nuts. Most people live with the problems."
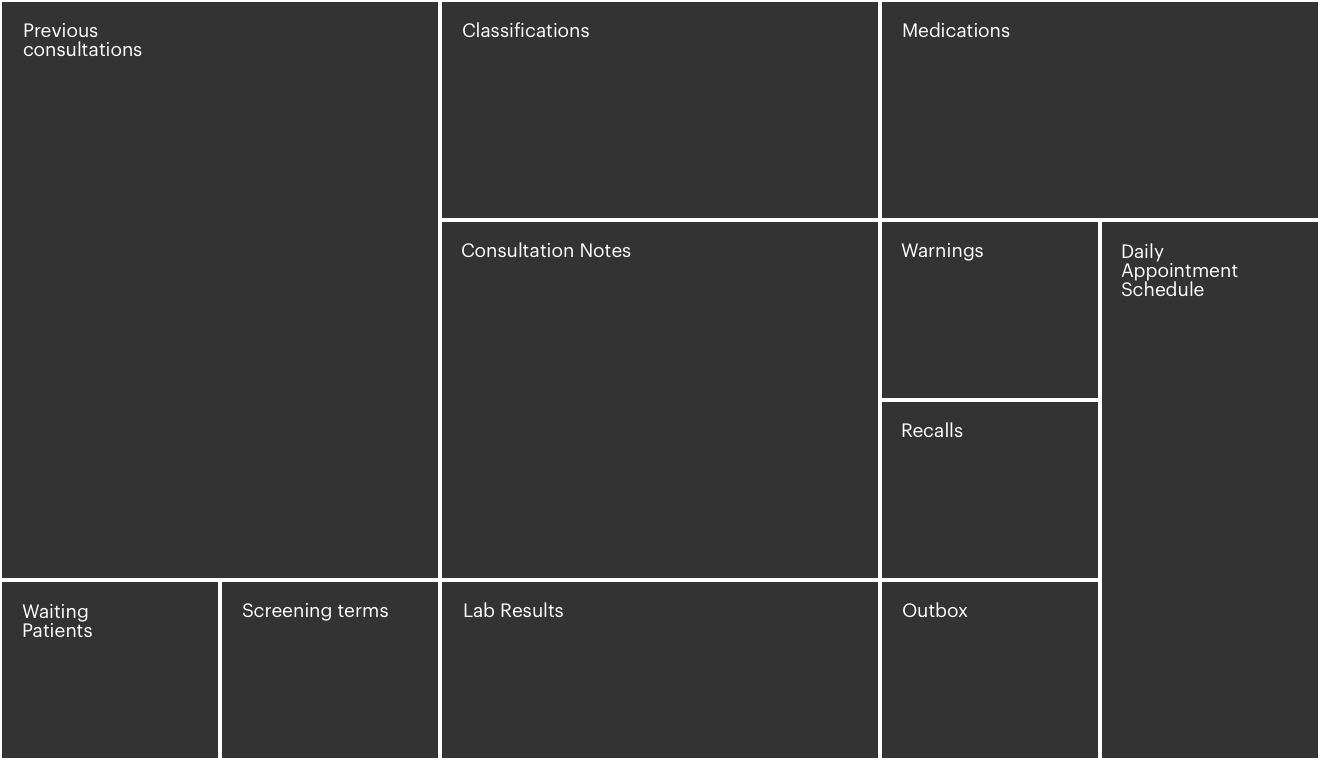
The diagram below is his arrangement, and he explained why this worked best, and how
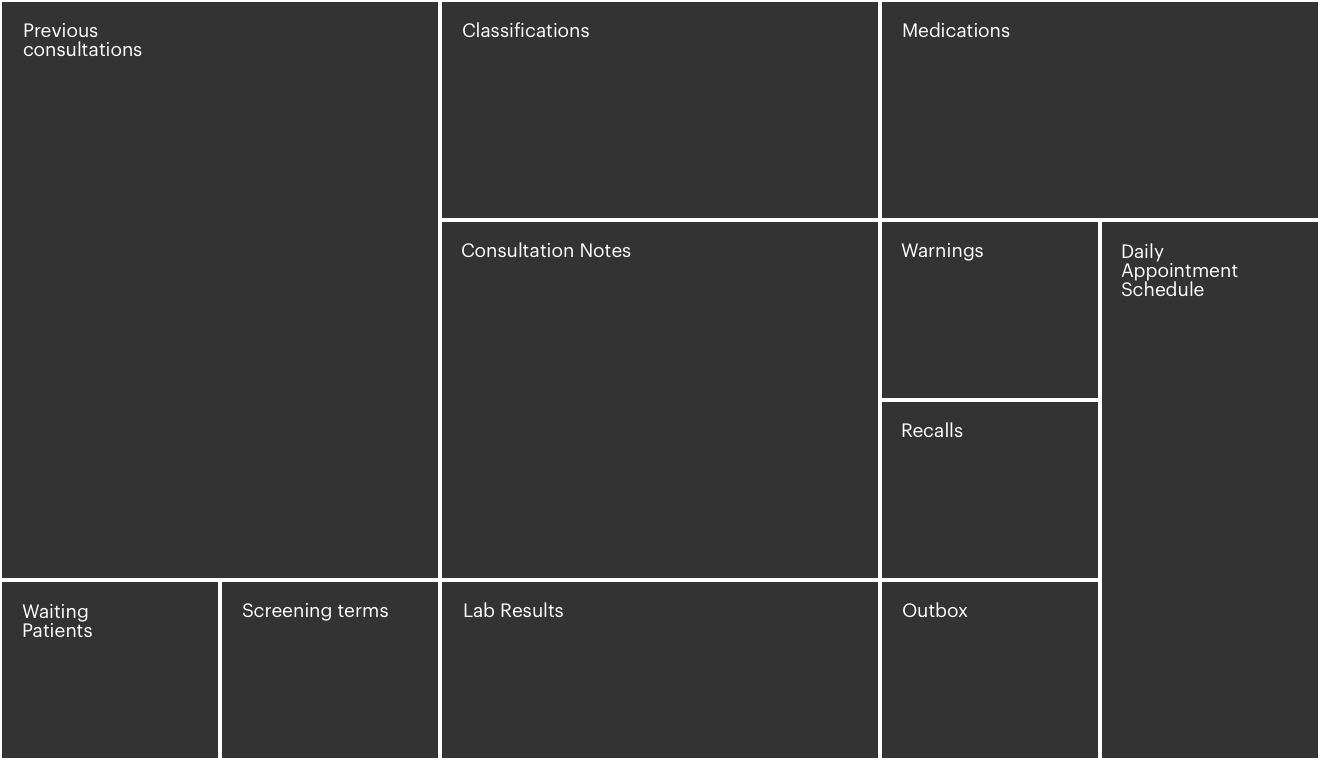
The consultation notes window is where he writes the notes for the patient he is treating. He puts it right at the centre of the monitor, to avoid distraction and stay focused.
He uses a structured template system for his notes - diagnoses, examination, history, plan. He specifically puts diagnosis right at the top of the note, as that will instantly tell him if he needs to read the rest of it when looking through past consultation notes. For example, he would read an annual review of a patient in more detail, than a viral cold. In traditional SOAP notes, the diagnosis (or assessment) is put 2/3rds down the notes, which he considered absolutely daft, and a waste of time.
The other very important part of his template is the plan - he always puts it at the bottom of the note, and lists actions in bullet points. That way it's always absolutely certain what the plan is - what he's done, when he's expecting improvement, and if needed when he'll see them again. He said many GPs would make notes which you can read that they came in with a chest infection, but it's just not clear what was done with them, or what the follow up was, or what safety netting was in place. Bryan believes good documentation is the cornerstone of good practice - for both the GP's protection, the patient's protection, and just good outcomes.
He's been using a formalised system since he came to NZ. He tries to tell a story, instead of abbreviated consultations, so if he reads something 3 years old, he can recall the consultation clearer. It's taken him 9 years to convince the other GPs at his practice to use it, but now everybody uses it by default. A compliment he has received from GP's who have tried his system is that it made them more conscious about what they're writing.
The classifications list is where you write down the major points of their medical history. He places it directly above the note as he needs to be constantly aware of their major medical conditions, and he needs to take it into consideration during day to day practice.
One critique he has of MedTech32, is that classifications cannot be ordered. Some classifications are simply more important - knowing a patient has had a stroke, or has heart disease is more important than knowing they had something less critical, such as a hernia repair. By the time a patient is significantly elderly, you might be obscuring the important classifications, with less important ones.
Patient classifications are sometimes called 'the problem list' by some GPs - which causes issues. Some GPs might add things such as, "Can't get out of the house", which isn't a medical condition. There is individuality in practices in how they work.
Directly next to the classifications, is the patient's medication list. It makes sense that next to their major medical conditions are the medications treating them.
The medication list needs to be broken up into long term, and short term medication. Short term is something prescribed for a one off condition, say antibiotics for a sore throat. Long term medication are medications taken regularly. It's important to separate the list, so it's readable, but also makes it hard to accidentally mess up renewing medication - either renewing something they should not have had, or missing a regular medication. Bryan also thinks a 'renew all' button is critical, instead of doing them one by one. If a patient is on 10 regular medications, that's 40 clicks a year.
MedTech provides warnings if you try to prescribe a patient a medication that they're allergic to, or that could interact with existing medication. Bryan has logically placed it beneath the medication window.
I asked him about obtrusive notifications, which alert with a popup. He said that in theory that's nice, but in practice you get patients with 25 notifications, and you end up by reflex just clicking through them - there's just too many to pay attention to. That is actually quite dangerous, as you might miss a really important notification. You're going to have so many reminders as a doctor - from other bodies as a pet project, that notifications really have to be configurable.
Recalls are planned future appointments, usually for annual reviews, cervical smears, retinal screening, or follow up after a consultation. This provides an overview for the patient's year.
Outbox is where documents are sent to other people on the patient's behalf, such as referrals to specialists.
Lab results are directly below the consultation note - this makes sense as the two most dominate pieces of info (classifications and lab tests) are closest to it.
"So if I suddenly see their sodium is 120, I think, I should do something for that"
Screening terms are quick references to things such as blood pressure, or cholesterol readings. These are usually entered in the main notes, but they enter them here as well, as they're faster to find than searching through consultation notes.
In Bryan's own words, if you want to make good medical software, "you need a fuckton of keyboard shortcuts". He avoids using the mouse as much as possible - setting up his own keyboard macros to customise the shortcuts that cannot be changed in MedTech32.
I asked him for his opinion on EHR systems, compared to the EMR system he was using. He noted that he remembered people trying to create working EHR systems when he was a medical student. He could absolutely see why centralised notes would be fantastic, but one of the downsides is notes where anybody can write anything - they end up being filled up with irrelevant information. So as much as it's useful, it can become distracting, hamper the other medical practitioner, and just simply not be safe.
He gave the example, that district nurses started using the screening terms window in MedTech32 to note that they've seen the patient. Which reduced the usefulness of that window for him. It's just not going to be relevant to a respiratory physician to know that the patient had constipation earlier in the year, or for him to know the full details of what a neurologist has been doing with a patient.
There needs to be a system to ensure only relevant information is shown, and that irrelevant information is hidden or quickly summarised.